ZOLADEX SafeSystem® is the only ready‑to‑use GnRH agonist1
ZOLADEX is designed for safe and efficient administration—no assembly, mixing, or refrigeration required
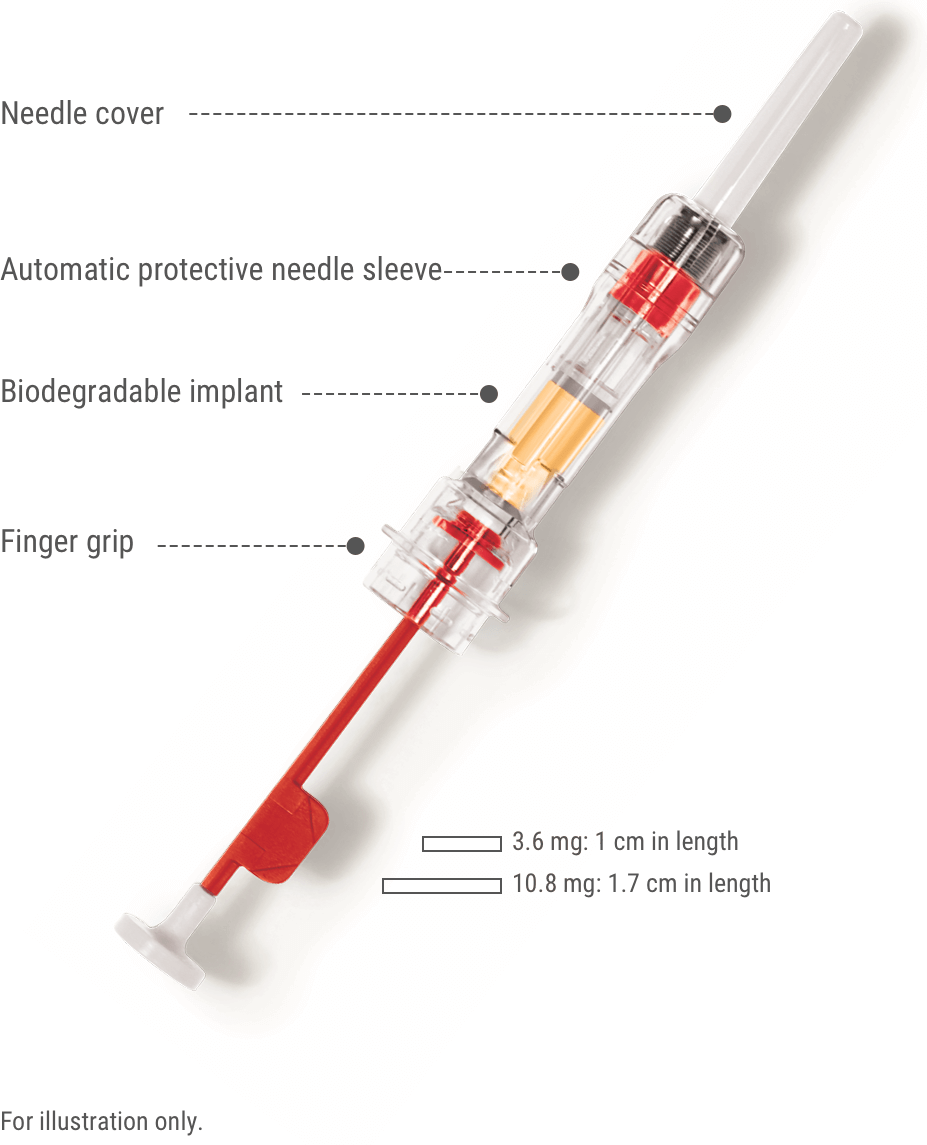
ZOLADEX features:
- A sterile, siliconized, triple-beveled hypodermic needle with easy-glide SafeSystem
- Implant provides consistent, reliable delivery of medication
- Each syringe is provided with a convenience pack (contains gauze, alcohol wipe, and bandage)
-
Designed with a protective needle sleeve to reduce needlestick injuries5
- ZOLADEX SafeSystem needle is automatically covered upon withdrawal
ZOLADEX helps meet the needs of nurses6,7
In a study with nurses, it took an average of 1.70 minutes to prepare and deliver ZOLADEX6
- Randomized, crossover study with 82 nurses timed in the administration (preparation and delivery) of the implant system used to administer ZOLADEX and the vial system used to administer leuprolide acetate. Preferences and perceptions of the ease of use and relative safety of the 2 injection systems were also assessed.6

The majority of patients reported minimal pain (VAS† <10 mm) from the ZOLADEX injection7
In a study with patients, there was no significant difference between the pain levels experienced from injections of ZOLADEX compared to injections of intramuscular leuprolide acetate7
- A total of 50 patients were blindfolded and administered either ZOLADEX or leuprolide acetate into the anterior abdominal wall. Each group (24 ZOLADEX and 26 leuprolide acetate) received 2 injections 4 weeks apart. Following each injection, patients were asked to record the pain of injection on a visual analogue scale ranging from 0 mm (no discomfort) to 100 mm (maximal discomfort).7
- †VAS: visual analogue scale.
ZOLADEX administration technique
PREPARATION: No refrigeration or premixing is required with ZOLADEX—the siliconized hypodermic needle with easy-glide SafeSystem comes ready to administer. You can also download this helpful guide for your office.
1. Prepare the patient:
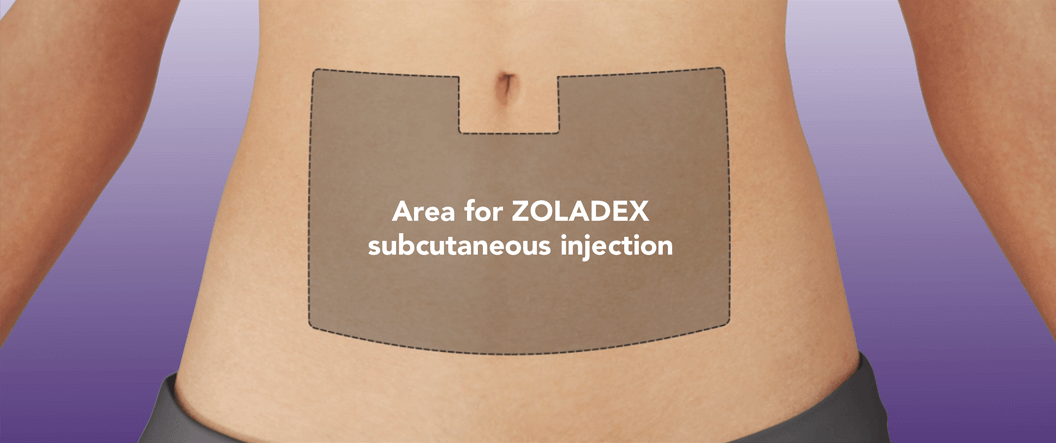
Put the patient in a comfortable position with the upper part of the body slightly raised. Prepare an area of the anterior abdominal wall below and two inches out from the navel line with an alcohol swab.
NOTE: Caution should be taken when injecting into the anterior abdominal wall due to the proximity of underlying inferior epigastric artery and its branches.
2. Prepare the injection:
Examine the foil pouch for damage, then open. Empty the pouch onto a counter or into your hand rather than pulling the syringe out of the pouch, as it is possible to inadvertently pull the plunger off of the syringe.
Hold the syringe at a slight angle to the light and confirm at least part of the ZOLADEX implant is visible. There is no need to remove air bubbles, like with liquid injections, and partially depressing the plunger prior to administration may cause the implant to fall from the syringe.
Gently peel the plastic safety tab up and away from the plunger and discard it. Remove the needle cover.
NOTE: If too much force is used when removing the plastic safety tab, the plunger can be pulled off.
3. Complete the injection:
Pinch the patient’s skin using aseptic technique at the prepared injection site. With the bevel of the needle facing up, grasp the protective sleeve of the syringe with the pointer finger, middle finger, and thumb.
Insert the needle subcutaneously at a 30- to 45-degree angle to the skin in one continuous, deliberate motion until the protective sleeve touches the skin.
NOTE: The ZOLADEX syringe cannot be used for aspiration. If the hypodermic needle penetrates a large vessel, blood will be seen instantly in the syringe chamber. If a vessel is penetrated, withdraw the needle and inject with a new syringe elsewhere. Monitor patients for signs or symptoms of abdominal hemorrhage.
Use extra care when administering ZOLADEX to patients with low BMI and/or patients receiving full dose anticoagulation.
While continuing to pinch the patient’s abdomen, move your fingers back to the syringe finger grip and place your thumb on the plunger. Grasping the syringe below the finger grip on the protective sleeve may prevent the protective sleeve from activating.
While grasping the finger grip, depress the plunger until you cannot depress it any further. This ensures the implant has been deposited in the correct location in the abdomen. Use sufficient force to depress the plunger, as a degree of resistance can be experienced.
After fully depressing the plunger, begin withdrawing the needle, and the SafeSystem protective sleeve will deploy to cover the syringe. The needle itself does not retract. Dispose of the syringe in an approved sharps collector.
Watch this helpful video for more information on how to administer ZOLADEX
Request in-office injection training by calling 1‑844‑ZOLADEX (1‑844‑965‑2339).
*For eligible, commercially insured patients, card carries a maximum of $300 per 1-month supply and $900 per 3-month supply with a maximum annual benefit of $2,000 per calendar year. You are not eligible if prescriptions are paid by any state or other federally funded programs, including, but not limited to, Medicare or Medicaid, Medigap, VA or DOD or TRICARE, or where prohibited by law.
- ZOLADEX® (goserelin implant) 3.6 mg. Prescribing Information. TerSera Therapeutics LLC.
- LUPRON DEPOT® (leuprolide acetate for depot suspension). Prescribing Information. AbbVie Inc.
- ELIGARD® (leuprolide acetate). Prescribing Information. Tolmar Pharmaceuticals Inc.
- TRELSTAR® (triptorelin pamoate for injectable suspension). Prescribing Information. Verity Pharmaceuticals, Inc.
- Moser MA. Engineering out needle stick injuries (safety devices). The Safe Angle. Summer 2004;5-7.
- Morgan G, Cooley C. Injection systems for two luteinising hormone-releasing hormone agonists: a comparative assessment of administration times and nurses’ perceptions. Eur J Oncol Nurs. 2005;9:334-340.
- Montgomery BS, Borwell JP, Higgins DM. Does needle size matter? Patient experience of luteinising hormone-releasing hormone analogue injection. Prostate Cancer Prostatic Dis. 2005;8:66-68.
- Taylor CW, Green S, Dalton WS, et al. Multicenter randomized clinical trial of goserelin versus surgical ovariectomy in premenopausal patients with receptor-positive metastatic breast cancer: an intergroup study. J Clin Oncol. 1998;16:994-999.
- De Vos FY, van Laarhoven HW, Laven JS, et al. Menopausal status and adjuvant hormonal therapy for breast cancer patients: a practical guideline. Crit Rev Oncol Hematol. 2012;84:252-260.
- Rossi L, Pagani O. Adjuvant endocrine therapy in breast cancer: evolving paradigms in premenopausal women. Curr Treat Options Oncol. 2017;18:28. doi:10.1007/s11864-017-0473-1.
- Im SA, Lu YS, Bardia A, et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. N Engl J Med. 2019;381:307-316.
- Loibl S, Turner NC, Ro J, et al. Palbociclib combined with fulvestrant in premenopausal women with advanced breast cancer and prior progression on endocrine therapy: PALOMA-3 results. Oncologist. 2017;22(9):1028-1038.
- VERZENIO® (abemaciclib). Prescribing Information. Eli Lilly and Company.
Important Safety Information
Anaphylactic reactions to ZOLADEX have been reported in the medical literature. ZOLADEX is contraindicated in patients with a known hypersensitivity to GnRH, GnRH agonist analogues, or any of the components in ZOLADEX.
ZOLADEX is contraindicated during pregnancy unless used for palliative treatment of advanced breast cancer. ZOLADEX can cause fetal harm when administered to a pregnant woman. If used during pregnancy, the patient should be apprised of the potential hazard to the fetus. There is an increased risk for pregnancy loss due to expected hormonal changes that occur with ZOLADEX treatment. ZOLADEX should not be given to women with undiagnosed abnormal vaginal bleeding.
Pregnancy must be excluded for use in benign gynecological conditions. Women should be advised against becoming pregnant while taking ZOLADEX. Effective nonhormonal contraception must be used by all premenopausal women during ZOLADEX therapy and for 12 weeks following discontinuation of therapy.
Transient worsening of tumor symptoms, or the occurrence of additional signs and symptoms of breast cancer, may occasionally develop during the first few weeks of treatment. Some patients may experience a temporary increase in bone pain. Monitor patients at risk for complications of tumor flare.
Hyperglycemia and an increased risk of developing diabetes or worsening of glycemic control in patients with diabetes have been reported in men receiving GnRH agonists like ZOLADEX. Monitor blood glucose levels and glycosylated hemoglobin (HbA1c) periodically and manage according to current clinical practice.
Increased risk of developing myocardial infarction, sudden cardiac death and stroke has been reported in association with use of GnRH agonists like ZOLADEX in men. Patients receiving a GnRH agonist should be monitored for symptoms and signs suggestive of development of cardiovascular disease and be managed according to current clinical practice.
Hypercalcemia has been reported in some breast cancer patients with bone metastases after starting treatment with ZOLADEX. If hypercalcemia does occur, appropriate treatment measures should be initiated.
Hypersensitivity, antibody formation and acute anaphylactic reactions have been reported with GnRH agonist analogues.
ZOLADEX may cause an increase in cervical resistance. Therefore, caution is recommended when dilating the cervix for endometrial ablation.
GnRH agonists may prolong the QT/QTc interval. Providers should consider whether the benefits of androgen deprivation therapy outweigh the potential risks in patients with congenital long QT syndrome, congestive heart failure, frequent electrolyte abnormalities, and in patients taking drugs known to prolong the QT interval. Electrolyte abnormalities should be corrected. Consider periodic monitoring of electrocardiograms and electrolytes.
Injection site injury and vascular injury including pain, hematoma, hemorrhage and hemorrhagic shock, requiring blood transfusions and surgical intervention, have been reported with ZOLADEX. Extra care should be taken when administering ZOLADEX to patients with low BMI and/or to patients receiving full dose anticoagulation.
Depression may occur or worsen in women receiving GnRH agonists.
Treatment with ZOLADEX may be associated with a reduction in bone mineral density over the course of treatment. Data suggest a possibility of partial reversibility. In women, current available data suggest that recovery of bone loss occurs on cessation of therapy in the majority of patients.
In women, the most frequently reported adverse reactions were related to hypoestrogenism. The adverse reaction profile was similar for women treated for breast cancer, dysfunctional uterine bleeding, and endometriosis.
The most commonly reported adverse reactions with ZOLADEX in clinical trials for endometriosis were: hot flashes (96%), vaginitis (75%), headache (75%), decreased libido (61%), emotional lability (60%), depression (54%), sweating (45%), acne (42%), breast atrophy (33%), seborrhea (26%), and peripheral edema (21%).
The most commonly reported adverse reactions with ZOLADEX in clinical trials for endometrial thinning were: vasodilation/hot flashes (57%), headache (32%), sweating (16%), and abdominal pain (11%).
The most commonly reported adverse reactions with ZOLADEX in breast cancer clinical trials were hot flashes (70%), decreased libido (47.7%), tumor flare (23%), nausea (11%), edema (5%), and malaise/fatigue/lethargy (5%). Injection site reactions were reported in less than 1% of patients.
For ZOLADEX 3.6 mg: Hot flashes (62%), sexual dysfunction (21%), decreased erections (18%), lower urinary tract symptoms (13%), lethargy (8%), pain (worsened in the first 30 days) (8%), edema (7%), upper respiratory infection (7%), rash (6%), and sweating (6%).
For ZOLADEX 10.8 mg: Hot flashes (64%), pain (general) (14%), gynecomastia (8%), pelvic pain (6%), and bone pain (6%).
In the locally advanced carcinoma of the prostate clinical trial, additional adverse event data were collected for the combination therapy with radiation group during both the hormonal treatment and hormonal treatment plus radiation phases of this study. Adverse experiences (incidence >5%) in both phases of this study were hot flashes (46%), diarrhea (40%), nausea (9%), and skin rash (8%). Treatment with ZOLADEX and flutamide did not add substantially to the toxicity of radiation treatment alone.
Indications
ZOLADEX 3.6 mg and ZOLADEX 10.8 mg
Management of locally confined Stage T2b-T4 (Stage B2-C) carcinoma of the prostate in combination with flutamide. Treatment with ZOLADEX and flutamide should start 8 weeks prior to initiating radiation therapy and continue during radiation therapy.
Palliative treatment of advanced carcinoma of the prostate.
ZOLADEX 3.6 mg
Management of endometriosis, including pain relief and reduction of endometriotic lesions for the duration of therapy. Experience with ZOLADEX for the management of endometriosis has been limited to women 18 years of age and older treated for 6 months.
Use as an endometrial-thinning agent prior to endometrial ablation for dysfunctional uterine bleeding.
Palliative treatment of advanced breast cancer in pre- and perimenopausal women.
To report suspected adverse reactions, contact the FDA at 1‑800‑FDA‑1088 or www.FDA.gov/medwatch. You may also contact TerSera Therapeutics at 1‑844‑334‑4035 or medicalinformation@tersera.com.
Please see Full Prescribing Information for ZOLADEX 3.6 mg and ZOLADEX 10.8 mg.